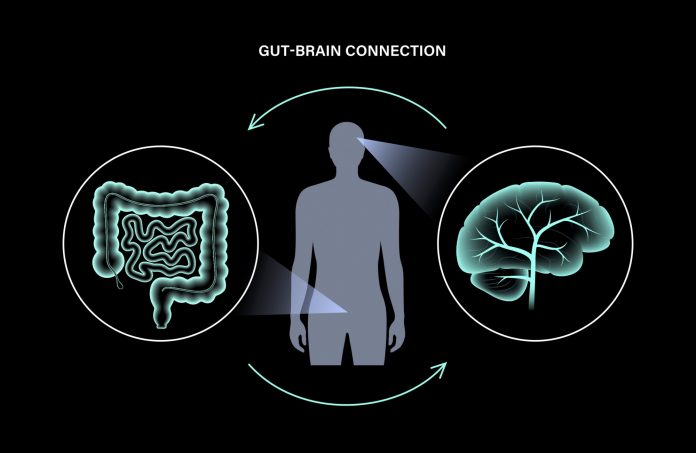
Much like a highway that connects a network of transport, the vagus nerve is the ‘highway’ that travels between the gut and the brain and is where information is transmitted from one to the other.
“The gut-brain axis is a combination of many communication pathways that are responsible for the transfer of information between our GI tract, the bacteria that live in our gut, and our brain,” said Dr Andrew Shoubridge, Postdoctoral Research Fellow in the Microbiome and Host Health Group at the South Australian Health and Medical Research Institute.
“These pathways are varied and diverse and can involve circulating cells from the immune system, hormones produced from intestinal cells, compounds such as neurotransmitters, produced from gut bacteria, and also direct neuronal communication between the gut and brain via the vagus nerve.
“The vagus nerve extends directly out of our brainstem – located at the base of our brain – all the way down our body, through our neck and chest to our lower abdomen.”
Dr Shoubridge adds that the vagus nerve is “one of the biggest nerves functionally”, with some of its functions, apart from this transmission of information between brain and gut, including the regulation of satiety, the digestion of food, and “reflexive actions such as coughing, sneezing, swallowing and vomiting”.
Given the intricate connection between the gut and the brain – the vagus connection – it’s no surprise that gut health, mental health and wellbeing are linked.
“There are many different types of microbes within our gut, which impact mental health in different ways,” Dr Shoubridge said.
“Some microbes produce neurotransmitters that directly affect neuronal growth and performance, while others produce compounds that can cause pro- or anti-inflammatory conditions within the body. Growth of these microbes is known to be impacted by what we eat and drink, but understanding the complete complexity of these relationships is an ongoing process.”
Addressing mental health specifically, Dr Shoubridge says the neurotransmitters produced by the gut that have the biggest effects are glutamate, gamma-aminobutyric acid (GABA), dopamine and serotonin.
“Glutamate and GABA are directly responsible for signals in the brain to travel from one neuron to another, and dopamine is involved in the reward/motivation circuit,” he said. “Serotonin is synthesised from the amino acid tryptophan and involved in multiple neuronal circuits, including mood and memory. Importantly, 95 per cent of the body’s tryptophan is produced in the gut.”
With this role of gut bacteria (the gut microbiome) in the production of neurotransmitters such as dopamine and serotonin, it’s important to keep the gut healthy to support the growth of these bacteria. In turn, this will have a positive effect on enhancing mental health and wellbeing.
“Our gut microbiome is affected by a vast range of factors that could be targeted to improve mental health and wellbeing,” Dr Shoubridge said.
Some of these factors, he advises, include smoking, alcohol consumption, medications, obesity and high-fat diets, which are known to adversely alter gut health and “have all been connected with mental health disorders and neurological diseases”.
“Studies are investigating these connections further to identify the best opportunities for health improvement,” he said.
One of the most influential factors affecting the gut microbiome is diet. Dr Shoubridge points to “latest research” that supports the benefits of a Mediterranean diet in this and other areas.
“The Mediterranean diet is best suited to improving the health of not only our gut, but also our cognition, mood and wellbeing,” he said, pointing to the diet’s emphasis on plant foods, being rich in fruit, vegetables, extra virgin olive oil, legumes, nuts and oily fish.
Dr Shoubridge also supports the intake of both pre- and probiotics in assisting the growth of a healthy gut microbiome.
“Prebiotics provide food for the healthy bacteria in the microbiome [while] probiotics contain live and healthy bacteria that aid in the positive health of the microbiome,” he said.
But he adds that, when it comes to mental health, information on the role that pre and probiotic treatments play is limited.
“While some benefits have been described, such as a reduction in dangerous inflammatory compounds that reach the brain, this is restricted to pre-clinical investigations, with the possible benefits for people not yet established,” Dr Shoubridge said. “Treatments that have seen more extensive research and success focus on dietary interventions.”
Addressing the role of pharmacists in assisting customers in optimising gut health and enhancing mental health and wellbeing, he recommends a focus on lifestyle and dietary interventions, including adopting a Mediterranean diet, achieving a healthy weight, stopping smoking, and reducing alcohol intake.
“Pharmacies can help in discussing some of these lifestyle choices, such as dietary changes, with their customers,” Dr Shoubridge said.
This feature was originally published in the August issue of Retail Pharmacy magazine.