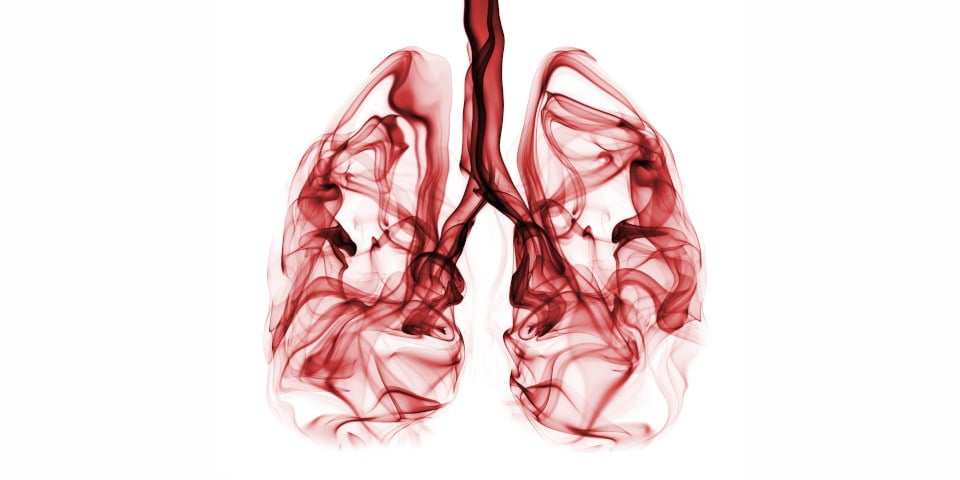
Lung cancer is Australia’s biggest cancer killer, responsible for 8693 deaths last year alone1. Despite such devastation, general awareness of the range of the disease’s causes is relatively low.
A number of factors can increase the risk of lung cancer: smoking, air pollution, family history, exposure to carcinogens at work, genetics and personal history of lung disease. While smoking is a significant factor – it’s estimated that 81 per cent of lung cancers in Australia in 2010 have been caused by tobacco smoking2 – it’s not the sole cause. Yet a perception remains among many that lung cancer is self-inflicted.
A survey conducted by Lung Foundation Australia (LFA) found that 35 per cent of Australians surveyed believe people living with lung cancer are their “own worst enemy,” who “have only themselves to blame.” One in 10 of those surveyed also believe that those with lung cancer “got what they deserved”.
“This judgement negatively impacts the perceived worthiness of people to access support and reduces their sense of entitlement to care and empathy,” the foundation highlights in its report into lung cancer reform, ‘The next breath: Accelerating lung cancer reform in Australia 2022-2025’.3
Something in the air
According to LFA, 20 per cent of people who are diagnosed with lung cancer have never smoked, with air pollution now being recognised as a serious risk factor.
Recent findings from the European Society for Medical Oncology (ESMO) help explain how air pollution causes lung cancer in people who have never smoked.4
The findings outline how fine particulate matter contained in car fumes and from burning fossil fuels “awakens” dormant mutations in lung cells and tips them into a cancerous state. The work helps explain why so many non-smokers develop lung cancer and is a wake-up call about the damaging impact of pollution on respiratory health.
“The same particles in the air that derive from the combustion of fossil fuels, exacerbating climate change, are directly impacting human health via an important and previously overlooked cancer-causing mechanism in lung cells,” said Charles Swanton, Principal Group Leader at the UK’s Francis Crick Institute and Cancer Research UK Chief Clinician, who presented the research results at the ESMO 2022 Presidential Symposium in September.
“The risk of lung cancer from air pollution is lower than from smoking, but we have no control over what we all breathe. Globally, more people are exposed to unsafe levels of air pollution than to toxic chemicals in cigarette smoke, and these new data link the importance of addressing climate health to improving human health.”
In addition to its impact on cancer incidence, air pollution is linked with respiratory impacts such as respiratory disease, decreased pulmonary function and respiratory infections, as well as heart disease and stroke.
Reform needed
Air pollution is the presence of one or more contaminants in the atmosphere, such as dust, fumes, gas, mist, odour, smoke or vapour.
In Australia, air pollution is putting a $16 billion strain on the economy each year, as well as contributing to 3000 premature deaths5 and direct health system costs specific to lung cancer amounting to more than $4 million annually.6
The World Health Organisation’s International Agency for Research on Cancer concluded in 2013 that outdoor air pollution is carcinogenic to humans, with the particulate matter component of air pollution most closely associated with increased cancer incidence, especially lung cancer.
In 2021, the WHO published new Air Quality Guidelines that outline evidence-based recommendations to help countries achieve safe air quality.7 Australia is yet to adopt these guidelines to reduce air pollution. As a result, this country is now falling behind with insufficient air quality standards that are putting the health of Australians at risk.
“This new publication reinforces the alarming findings from the [federal government’s] ‘Australia State of the Environment 2021’ report that was made public in July this year,” LFA CEO Mark Brooke said.
“The environment and health are intrinsically linked, and we need all levels of government to acknowledge the burden that poor air quality has on all Australians, and commit to action, as well as considering the additional challenges that the one in three Australians who are living with a pre-existing lung condition face.”
LFA reinforces the need for a ban on backyard fire pits and the replacement of out-of-date wood heaters and stoves to minimise air pollution in residential areas.
The foundation is also calling on the federal government to set clear targets and actions, develop a national strategic action plan for air quality, and adopt the WHO Air Quality Guidelines, to help protect health and ensure clean air for Australia.
“Lungs are made to breathe clean air, and the environments where we work, live and play have a significant short- and long-term impact on health,” the LFA report stated.
“Air pollutants are often invisible, so it is important Australia does not become complacent and instead should take a more proactive approach to protect health and ensuring good air quality.”
References
- Australian Institute of Health and Welfare. ‘Cancer in Australia 2021’. Cancer series no. 133. Cat. no. CAN 144. Canberra: AIHW; 2021.
- Pandeya N, Wilson LF, Bain CJ, Martin KL, Webb PM, Whiteman DC. ‘Cancers in Australia in 2010 attributable to tobacco smoke’. Aust NZ J Public Health, 2015; 39 (5): 464-70.
- lungfoundation.com.au/wp-content/uploads/2022/08/OYO220615_LFA_Lung-Cancer-Blueprint-2_Digital.pdf
- Research presented at the ESMO Congress 2022. LBA1 – ‘Mechanism of action and an actionable inflammatory axis for air pollution-induced non-small cell lung cancer: Towards molecular cancer prevention’. Annals of Oncology, 2022; 33 (suppl_7): S808-S869. 10.1016/annonc/annonc1089.
- Hanigan IC, Broome RA, Chaston TB, Cope M, Dennekamp M, Heyworth JS et al. ‘Avoidable mortality attributable to anthropogenic fine particulate matter (PM 2.5) in Australia’. Int J Environ Res Public Health, 2020; 18 (1).
- Australian Institute of Health and Welfare. ‘Health system expenditure on cancer and other neoplasms in Australia, 2015-16’. Cancer series no. 131. Cat. no. CAN 142. Canberra: AIHW; 2021.
- ncbi.nlm.nih.gov/pmc/articles/PMC8494774/
This feature was originally published in the November issue of Retail Pharmacy magazine.