Polycystic ovarian syndrome (PCOS) is a common hormonal condition that affects one in 10 women of reproductive age1, and up to 13 per cent of all women2, yet it’s also considered a “neglected condition”.2
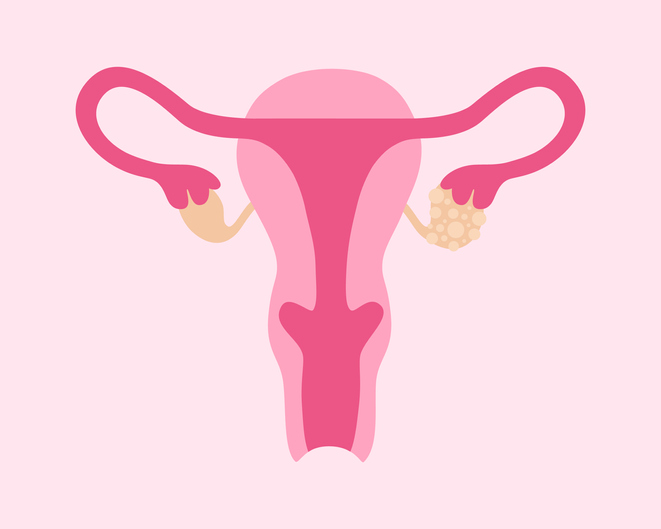
Being a hormonal condition, PCOS affects many parts of the reproductive system and can cause disruption to a woman’s “menstrual cycle, skin and hair, as well as causing cysts to develop on the ovaries”.1 According to Healthdirect, PCOS is “one of the leading causes of infertility, yet many people don’t know they have it – many females with PCOS aren’t diagnosed”.1
No cure for this condition currently exists, making effective management crucial. One of the aims of PCOS management is health outcome control, which often includes diet and healthy lifestyle advice, plus counselling support, as well as guidance around appropriate medications to manage fertility issues and surgery.3
PCOS signs and symptoms
The signs and symptoms of PCOS may vary between women, but typically include:
- Irregular periods or no periods.
- Hair growth on face, stomach and back.
- Loss or thinning of scalp hair.
- Acne that can be severe.
- Weight gain.
- Emotional problems (anxiety, depression, poor body image).
- Difficulties becoming pregnant.
- Increased risk of type 2 diabetes, with earlier onset.3
New international PCOS guidelines
Given its wide-ranging health effects, effective PCOS management often requires a multidisciplinary approach and up-to-date management guidelines for health professionals to follow.
To improve the lives of those living with PCOS, a Monash University-led partnership has developed international guidelines: the ‘2023 International Polycystic Ovary Syndrome Guidelines’.
These include recommendations for diagnosis, lifestyle, wellbeing, fertility and treatment, as well as improved care and support. They aim to address the priority needs of those with PCOS and are supported by significant freely available resources for women and their healthcare providers, to optimise health outcomes. They also address the need for new approaches to care, personalised healthcare experiences, evidence-based therapies, and optimised pregnancy care.
Monash University’s Professor Helena Teede, a leading global academic in PCOS and the driving force behind the new guidelines, says they highlight priority areas such as higher weight gain, diabetes and heart disease risk, and effective treatments, including those for infertility.
“The guidelines bust myths around higher weight and lifestyle and seek to support those with PCOS and reduce stigma,” she said. “Australians are exposed to an environment that drives rapid weight gain due to failures in policy, regulation and financial constraints, with women with PCOS at even higher risk.
“The focus is often on ineffective individual behavioural solutions, further impacting health and fertility. Limited access to effective therapies and fertility services leaves women with poorer health outcomes, especially [those in] underserved populations, presenting a health equity issue.”
The new PCOS guidelines aim to deliver timely diagnosis, accessible information and education, support, and optimal models of care. They also aim to enhance healthcare professional education, awareness and support, while fostering partnerships and shared decision-making with those affected by PCOS globally.
For more information and to access the guidelines, visit:
References
- healthdirect.gov.au/polycystic-ovarian-syndrome-pcos
- racgp.org.au/newsgp/clinical/pcos-guidelines-shine-light-on-neglected-condition
- jeanhailes.org.au/resources/pcos-fact-sheet
Full Article availalble in Retail Pharmacy December magazine